Psoriasis is more than a skin condition. It consists of chronic inflammation that can affect the eyes, joints, and gastrointestinal (GI) tract, among other areas.
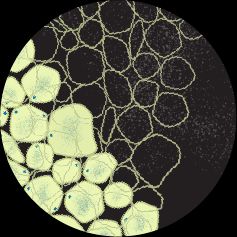
Psoriasis is a dermatological condition featuring areas of thickened or raised skin often covered in silvery-white scales. These patches can appear red or pink on lighter skin tones, while darker skin tones may take on a brown or purple hue.
While several types of psoriasis exist, plaque psoriasis is the most common, affecting approximately 80—90% of people living with psoriasis.
Skin manifestations are the most obvious symptoms of psoriasis, but inflammation from this condition can have body-wide effects.
This article discusses what happens to the body during psoriasis flare-ups, which are periods of time when symptoms of psoriasis suddenly or unexpectedly worsen.
Psoriasis affects more than just the skin. It is associated with eye, joint, and GI complications and may contribute to an increased risk for other chronic conditions, such as cardiovascular disease.

Eye complications
According to a 2021 review, the main eye complications associated with psoriasis
- Keratoconjunctivitis sicca: dry eye syndrome
- Blepharitis: eyelid inflammation
- Conjunctivitis: inflammation of the conjunctiva, the clear layer over the white of the eye
- Uveitis: inflammation of the uvea, the middle layer of the eye
Joint complications
Psoriasis is part of psoriatic disease, a broader term that includes the condition of psoriatic arthritis (PsA). Psoriasis and PsA are separate conditions, but because they are commonly seen together and
Research estimates
Psoriasis is also associated with axial spondyloarthritis (axSpA), inflammation affecting the spine and pelvis. Although it is unclear if psoriasis contributes to axSpA development or vice versa, an observational study from 2023 notes
GI complications
Psoriasis may contribute to inflammatory bowel disease (IBD), which includes Crohn’s disease and ulcerative colitis.
According to a 2022 review, people living with psoriasis have a
Other digestive symptoms, such as pain, bloating, fullness, and diarrhea, are common in psoriasis. These symptoms are attributed to how chronic inflammation affects gut permeability, the rate at which the lining of the GI tract allows substances to pass through into the bloodstream.
Too-high gut permeability can trigger immune responses throughout the body, which experts think contributes to many immune-mediated conditions such as celiac disease and type 1 diabetes.
Inflammation underlies psoriasis and its other effects on the body.
While the exact causes of psoriasis are not clear, it does not start and end with the skin. Psoriasis is immune-mediated, which means overactive immune responses play a major role in why skin cells experience dysfunction.
Immune-mediated conditions, which include autoimmune diseases, create persistent inflammation in the body. Inflammation is a key part of the natural immune response. It helps increase blood flow and vessel permeability, allowing immune cells to quickly reach their destinations.
In psoriasis and other conditions where immune function is overactive, the inflammatory process becomes chronic. Long-term inflammation leads to an overabundance of inflammatory substances, such as cytokines, in the body. Over time, these substances can cause tissue damage, contributing to other disease processes.
Cytokines — proteins responsible for regulating the immune response — sustain overactive immune activity, which creates more cytokines, leading to a continuous cycle.
Certain cytokines, such as interleukin (IL)-17, have been linked to immune-mediated skin conditions, including psoriasis. According to a
Why do symptoms worsen during a psoriasis flare?
A psoriasis flare, or flare-up, is a period of time when symptoms worsen, often suddenly and without warning.
Flare-ups are due to triggers that exacerbate the inflammatory response already occurring in the body. Examples of triggers include:
- stress
- injury or irritation
- alcohol use
- smoking
- weather extremes
- infection
- medication
A psoriasis flare affects the body in the same way as psoriasis — by causing inflammation. Symptoms worsen because the trigger creates an additional inflammatory reaction, compounding existing inflammation.
Chronic inflammation is associated with an increased risk for certain co-occurring conditions known as comorbidities.
Common comorbidities in psoriasis include:
- Cardiovascular disease (CVD): Conditions affecting the heart and blood vessels, such as coronary artery disease, stroke, and heart failure.
- Metabolic syndrome: A combination of conditions known to increase the risk for serious health complications like diabetes, stroke, and CVD. Common factors
include :- excess abdominal fat
- high blood pressure
- elevated blood sugar
- high blood triglycerides
- low HDL cholesterol
- Obesity: Excessive body fat accumulation that poses a risk to health. Defined by the
World Health Organization (WHO) as a body mass index of over 30. - Type 2 diabetes: Caused when the body becomes resistant to insulin or does not make enough insulin.
- Depression: A mental health disorder featuring depressed mood, low energy, and loss of self-motivated activity.
- Anxiety: A natural feeling of anticipation, worry, or unease that, when persistent, can lead to an anxiety disorder, such as generalized anxiety disorder.
- Lung disease: Conditions that affect the airways and lung tissues,
specifically: - asthma
- chronic obstructive pulmonary disease (COPD)
- obstructive sleep apnea
- pulmonary hypertension
For most people, psoriasis is a lifelong condition. Treatment can improve symptom severity and frequency. Remission — the absence of all symptoms —
Treating psoriasis early on can help reduce the complications and co-occurring conditions associated with chronic inflammation.
Psoriasis is an immune-mediated condition associated with chronic inflammation. While its primary symptoms involve the skin, it can have widespread effects on other areas of the body.
Treatment can improve the symptoms of psoriasis and can reduce the chances of experiencing complications from chronic inflammation.