A pacemaker can greatly improve daily life, and many people can return to normal life quickly. However, it is important to maintain the device and be aware of certain lifestyle changes.
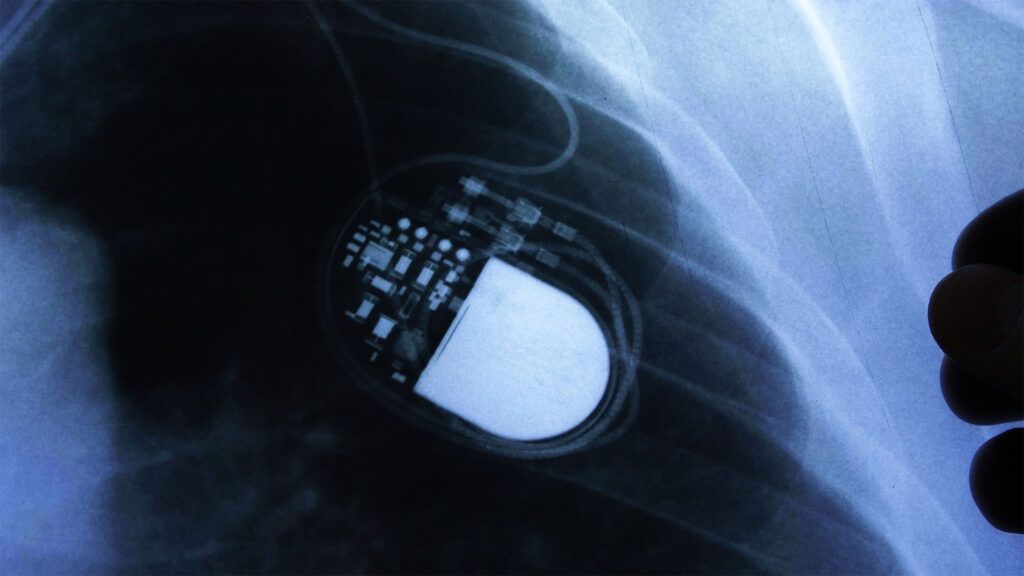
A pacemaker is a small device that helps the heart beat in a regular rhythm. A person may require a pacemaker if their heart rate is too fast or too slow.
A pacemaker connects to the chambers of the heart through tiny wires. It generates electrical impulses to help control irregular heart rates.
After having a pacemaker implanted, people may have concerns about getting on with their lives.
When people follow their doctor’s recommendations about daily activities, attend regular checkups, and maintain the device, they can continue living a normal and fulfilling life.
Pacemakers can help treat certain heart conditions, such as arrhythmias. As such, these devices can help support the heart, prevent life threatening conditions, and enable a person to live a regular life.
However, people may have concerns about having a pacemaker. It may take some time to become familiar living with one.
Some individuals might feel the pacemaker working. If this is the case, they can inform their doctor, who can change the settings.
Some people may also feel uncomfortable lying in certain positions or wearing certain clothes. However, this will not damage the pacemaker or affect how it works.
If a person has any concerns, they can discuss them with their care team. As a person becomes familiar with their pacemaker, it is important to remember that the pacemaker is helping the heart beat normally. As such, they should be safer with it than without it.
Read on to learn more about what to expect during pacemaker surgery recovery.
It is important to pay close attention to any changes or unusual patterns in a person’s pacemaker. The
- Knowing when to change the battery: Pacemakers are battery-powered, so the batteries will eventually need to be replaced. The batteries typically last for
6 to 15 years . A doctor will check the battery during appointments. If they believe the battery will start running out, they will perform a small operation to replace it. - Knowing what to do if it stops working: If the battery is running low or another part of the device is not functioning, it may need replacing or repair. If a person thinks their pacemaker may not be working, or they feel short of breath, dizzy, or faint, they should contact their doctor immediately.
- Software updates: A person can consult their doctor about how to regularly check for software updates.
- Watching for signs of infection: Chills, fever, and pain or redness at the site of the pacemaker may indicate an infection.
- Knowing your options and rights: A person has the right to request doctors turn off the pacemaker or remove it if they no longer think it is beneficial. A person may consider this if they are seriously ill or nearing the end of life. They can discuss their options and plans with their healthcare team.
If a person is unsure whether their pacemaker is functioning correctly, they can contact their doctor.
It is essential for a person to
A doctor will monitor the individual’s general health, check medications are working, and ensure the pacemaker is in optimal working condition.
A doctor may also advise contacting them to help with reprogramming the pacemaker as well as discussing any available software updates and upgrades.
Between visits, a doctor can also check the battery and wires are still working.
After a surgeon implants a pacemaker, a person should follow their doctor’s guidelines for recovery. The recovery period may take up to 6 weeks. During this time, it is advisable to avoid certain activities, such as:
- reaching up on the side of the operation
- strenuous activities
- driving
After recovering, there is no reason why living with a pacemaker should get in the way of a person’s social life.
However, it is important to try and reduce the risk of potential complications. For example, while health experts encourage physical activity, they
Within the first 12 months of having the device, a person is at a higher risk of infection. In some cases, this can lead to a rare complication known as endocarditis. It involves inflammation of the heart lining, most often the heart valves.
People should also be aware of a rare complication known as
Because a pacemaker is a battery-operated device that produces electrical impulses, it may be sensitive to other electrical devices or those with strong magnetic fields.
These devices may stop a pacemaker from working correctly, which can be difficult to identify.
Everyday devices
The
- cellphones
- tablets
- electronic cigarettes
- headphones
Certain household appliances, such as microwaves, should be safe to be near if they are working properly.
If a person suspects a device is disrupting their pacemaker, they should step away from it. A person can consult their doctor for further advice about what equipment to avoid.
Work and other venues
Many venues, such as shops or airports, may have security gates or metal detectors. Generally, these devices should not interfere with a pacemaker, but a person should move away from them after passing through.
However, certain handheld scanners at airports use strong magnets. As such, when passing through airport security, a person can show their pacemaker ID and ask for a hand search instead.
It is also worth noting that because metal detectors may identify a pacemaker, it is important to carry a pacemaker ID card to show to security guards.
Certain work environments may also not be suitable due to equipment generating electromagnetic fields. If a person has any concerns, they can contact their employer’s health and safety team or human resources.
Medical procedures
Additionally, it is important to inform healthcare professionals of a pacemaker before certain procedures. For example, a MRI scan uses a strong magnetic field to create detailed images, which could interfere with the functioning of a pacemaker.
The effects of medical equipment can vary depending on the type of pacemaker. A person can show their doctor or dentist their pacemaker ID card. The healthcare professional can advise whether the procedure is suitable and make the necessary changes if it is not.
When living with a pacemaker, a person should contact their care team if they experience the
- chest pain
- difficulty breathing
- sudden weight gain
- swelling in the legs and ankles
- fainting or dizzy spells
- hiccups that do not go away
Additionally, health experts recommend that a person carry a pacemaker ID card, bracelet, or necklace. This ensures that emergency personnel can identify that a person has a pacemaker in emergency situations.
The American Heart Association provides a printable download for a pacemaker wallet ID card
A pacemaker is a device that helps the heart beat at a regular rhythm. After recovering from implanting the device, most people can continue living a rich and fulfilling life. Typically, there is no need to make drastic changes to day-to-day life.
However, it is important for a person to regularly attend doctors’ appointments and know the signs that the pacemaker is no longer working. It is also advisable to carry a pacemaker ID card, bracelet, or necklace on their person.
