The autoimmune protocol (AIP) diet is an elimination diet intended to calm inflammation in the body. Although research is limited, it may hold benefits for people living with immune-mediated inflammatory conditions such as psoriasis.
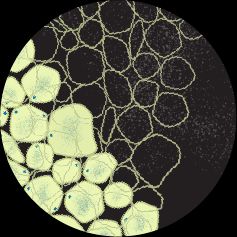
Psoriasis is an immune-mediated skin condition that causes patches of thickened, scaly skin. These patches can appear red and silvery on lighter skin or purplish-brown and gray on darker skin. While a handful of psoriasis types exist, plaque psoriasis is the
For reasons that health experts do not yet fully understand, an overactive immune response in psoriasis puts the body in a state of widespread inflammation. This triggers skin cells to multiply more quickly and causes other symptoms such as pain, nail bed changes, and dry skin.
As a way to help manage systemic inflammation, doctors may recommend an elimination diet such as the autoimmune protocol (AIP) diet to supplement current treatment strategies.
This article looks at the use of the AIP diet in psoriasis and the evidence behind it.
The AIP diet
“The premise of this diet, along with numerous other diets, is the bigger bucket idea of reducing inflammation in the body, as inflammation is a driver behind numerous inflammatory diseases, including psoriasis,” explained Dr. David Li, a board certified dermatologist from Boston, Massachusetts.
Different variations of the AIP diet exist in literature, but most involve the elimination of:
- grains
- legumes (beans, lentils, etc.)
- nightshade vegetables (tomatoes, peppers, eggplants, etc.)
- dairy
- eggs
- coffee
- alcohol
- nuts and seeds
- refined sugars
- processed oils
- food additives, including some spices
In the treatment of immune-mediated conditions, healthcare professionals use the AIP diet as an
After the elimination phase may come a maintenance phase, during which a person keeps their diet consistent for a period of time while focusing on developing a routine with alternative nutrient-dense foods.
Eventually, a person enters the reintroduction phase, in which they can reintroduce, one by one, the foods that they removed from their diet. During this time, a person and their doctor will closely monitor their symptoms for changes. If the reintroduction of a food correlates with an uptick in symptoms, the person and their doctor may permanently identify that food as a trigger.
Healthcare professionals use the AIP diet in immune-mediated conditions, including autoimmune conditions, to help manage systemic inflammation. Its premise comes from the
The GI tract contains
This link between the GI system and the immune system allows reactions of the GI tract to initiate systemic immune responses that can lead to inflammation in other parts of the body.
According to a
A hyperpermeable intestinal lining could allow inflammatory food triggers to pass through the barrier, creating an immune reaction that underlies certain immune-mediated conditions.
The authors of a
Very limited research exists on the use of the AIP diet, specifically, in psoriasis. But research does expand on the relationship between psoriasis and anti-inflammatory diet approaches.
For example, a
In a
But eliminating foods that promote inflammation is just one half of the whole anti-inflammatory diet approach. Including foods that may prevent inflammation is also a key point, according to some research.
A
The authors of a
Research remains limited overall, but researchers have studied the AIP diet more in certain immune-mediate conditions, such as inflammatory bowel disease (IBD). Ulcerative colitis and Crohn’s disease are types of IBD.
For example, a
Findings from a
A small
Health experts
“It’s important that patients realize that medications for psoriasis are more effective than diet modification alone and that this is not a mutually exclusive approach,” Li said. “It would be difficult to imagine recommending a diet alone to treat psoriasis, rather than evidence-based treatments with robust evidence for body surface area clearance.”
He cautioned that the AIP diet is not currently a common recommendation among dermatologists, even as a supportive therapy.
“[…] treatments are much more targeted now, whereas a diet may be a less targeted approach to reduce background inflammation. For instance, throughout my training and practice, I have only seen this diet being utilized 1–2 times.”
While the AIP diet can be nutritionally sound when a person has professional guidance in following it, Li pointed out that, to reduce any risk of medication interactions, it is important to consult with a doctor before starting the diet.
The AIP diet is an elimination diet that healthcare professionals use for supportive treatment of immune-mediated conditions. While research is limited, this diet may offer benefits for some people living with psoriasis.
Although the AIP diet is nutritionally sound, speaking with a doctor before starting this diet can help a person reduce the risk of medication interactions or other negative effects.